Salvaging Mangled Upper Limbs With Early Soft Tissue Cover With Flaps- A Case Series
Abstract
Summary
Mutilating upper limb injuries present complex challenges to both patients and surgeons, necessitating prompt and effective management strategies to achieve favorable outcomes. This retrospective study examines the cases of five consecutive patients with mangled upper limbs resulting from blunt trauma, evaluating demographics, injury mechanisms, injury patterns, and 60-day limb salvage outcomes. Among 2128 admissions between January and December 2022, five patients were identified with mangled upper limbs and open fractures, with an average age of 40.2 years and a notable male predominance (80%). The dominant hand was affected in 60% of cases, primarily due to blunt high-velocity road traffic accidents. The mean Mangled Extremity Severity Score (MESS) was 7.2, and the Ganga Hospital Open Injury Score averaged 16, indicating substantial injury severity without limb ischemia or compartment syndrome. All patients underwent definitive surgery within 48 hours, with various soft tissue reconstruction techniques employed, including free flaps, pedicle flaps, and local muscle mobilization, along with nerve grafting procedures. At the 60-day follow-up, successful limb salvage was achieved in all cases, with no instances of surgical site infection and excellent acceptance of skin grafted areas exceeding 95%. The findings underscore the importance of timely surgical intervention and comprehensive soft tissue coverage in achieving successful limb salvage outcomes in patients with mutilating upper limb injuries, emphasizing the critical role of early intervention and multidisciplinary collaboration.
Article
Salvaging mangled upper limbs with early soft tissue cover with flaps- A case series.
Authors;
Oshan Basnayake1,2, Dishan Samarathunga2, Pathum Abeysekara2, Paheerathan Nadesan2, Sameera Wijayawardhana2,3, Gayan Ekanayake2, Thushan Beneragama2, Dammika dissanayake2
1 Department of Anatomy, Genetics and Biomedical informatics, University of Colombo, Sri Lanka
2 Plastic and Reconstructive Surgical Unit, National Hospital of Sri Lanka, Colombo, Sri Lanka
3Department of Anatomy, Faculty of Medicine, University of Kelaniya
Correspondence to:
Oshan Basnayake
Lecturer, Department of Anatomy, Genetics and Biomedical informatics, Faculty of Medicine, University of Colombo, Sri Lanka
Email: oshan@anat.cmb.ac.lk
ORCID- https://orcid.org/0000-0002-1239-7506
Address: Department of Surgery, Faculty of Medicine, Kynsey Road, Colombo 8, Western Province, Sri Lanka
Tel – 0718 446 557
Fax – 94 – 112689135
DOI; https://doi.org/10.62474/GZPA7784
Summary
Mutilating upper limb injuries present complex challenges to both patients and surgeons, necessitating prompt and effective management strategies to achieve favorable outcomes. This retrospective study examines the cases of five consecutive patients with mangled upper limbs resulting from blunt trauma, evaluating demographics, injury mechanisms, injury patterns, and 60-day limb salvage outcomes. Among 2128 admissions between January and December 2022, five patients were identified with mangled upper limbs and open fractures, with an average age of 40.2 years and a notable male predominance (80%). The dominant hand was affected in 60% of cases, primarily due to blunt high-velocity road traffic accidents. The mean Mangled Extremity Severity Score (MESS) was 7.2, and the Ganga Hospital Open Injury Score averaged 16, indicating substantial injury severity without limb ischemia or compartment syndrome. All patients underwent definitive surgery within 48 hours, with various soft tissue reconstruction techniques employed, including free flaps, pedicle flaps, and local muscle mobilization, along with nerve grafting procedures. At the 60-day follow-up, successful limb salvage was achieved in all cases, with no instances of surgical site infection and excellent acceptance of skin grafted areas exceeding 95%. The findings underscore the importance of timely surgical intervention and comprehensive soft tissue coverage in achieving successful limb salvage outcomes in patients with mutilating upper limb injuries, emphasizing the critical role of early intervention and multidisciplinary collaboration.
Key words: upper limb injuries, limb salvage, soft tissue reconstruction, free tissue transfer, case series.
Introduction
Mutilating upper limb injuries are a major impact of patient as well as a challenge to the operating surgeon. Loss of function leads to loss of productive contribution to society. The ability to restore structure and function depends on the facilities and the expertise of the center of concern. Here we describe two mutilating upper limb injuries which we managed to get a good functional outcome.
Case details
Among 2128 admissions between January and December 2022, 5 patients were presented with severely injured upper limbs characterized by open fractures (Table 1). These individuals had an average age of 40.2 years, ranging from 28 to 54, with a male predominance (4 males, 80%). The dominant hand was affected in 60% of cases, and all injuries were attributed to blunt high-velocity road traffic accidents.
Table 1
Patient demographics, Mangled Extremity Severity Scores (MESS), and Ganga Hospital Open Injury Scores (GHOIS) and type of soft tissue cover used.
Abbreviations-ALT flaps; antero-lateral thigh flap, LD flap; Latissimus dorsi flap
|
Patient No |
Age(years), Gender | MESS | GHOIS | Soft tissue cover |
|
1 |
34 (Male) | 7 | 16 | Free ALT Flap |
|
2 |
28 (Male) | 7 | 17 | Free ALT Flap |
|
3 |
54 (Female) | 8 | 15 |
Pedicle LD Flap |
|
4 |
39 (Male) | 7 | 15 |
Skin graft |
| 5 | 46 (Male) | 7 | 17 |
Free ALT Flap |
Upon evaluation, the mean Mangled Extremity Severity Score (MESS) was 7.2, with a range of 7 to 8, indicating non salvageable limb injury. The Ganga Hospital Open Injury Score averaged 16, ranging from 15 to 17, reflecting the extent of tissue damage without evidence of limb ischemia or compartment syndrome. Within a critical window of 48 hours, all patients underwent definitive surgical interventions to address their injuries.
The surgical approach varied among the patients, with three individuals requiring free flap procedures, specifically antero-lateral thigh (ALT) flaps, while one patient received a pedicle latissimus dorsi flap (Figure 3), and another underwent local muscle mobilization and skin grafting for soft tissue coverage. Additionally, two patients underwent nerve grafting, with an average graft length of 9.5 cm.
After a 60-day follow-up period, all patients demonstrated successful limb salvage outcomes, characterized by the absence of surgical site infections and excellent acceptance rates exceeding 95% for skin grafted areas. These findings underscore the effectiveness of timely and comprehensive surgical management in achieving favorable outcomes in cases of severe upper limb trauma.
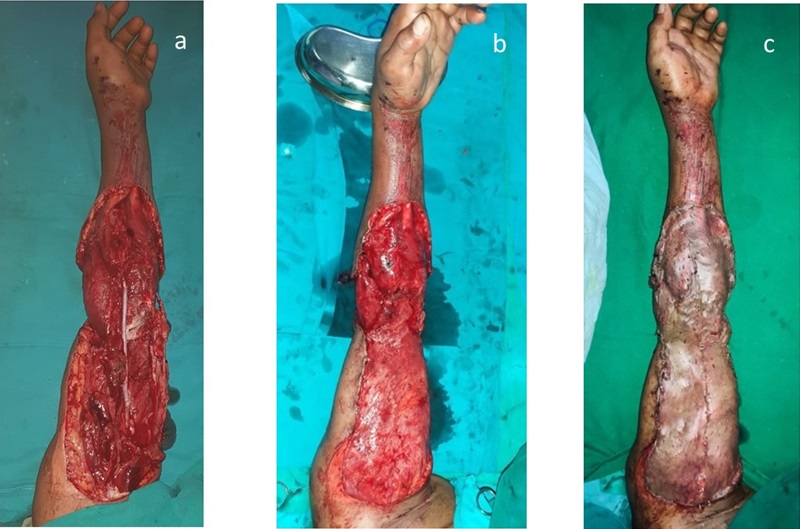
Apart from free ALT flap, patient 1 underwent a free toe transfer from 2nd toe to right thumb reconstruction and after 1 year, he has regained 3 types of grips of the hand (figure 1). Patient 2 had an open elbow joint where reconstruction of capsule and ulnar collateral ligament repair was performed with tensor fascia lata graft (Figure 2).
Figure 1- Patient 1- a. severely contaminated upper limb, b. appearance after wound debridement, c. after soft tissue cover with Free ALT flap and skin grafting, d. 6 months post-op after free flap and 2nd toe to thumb transfer

Figure 2- Patient 2- a. Pre-op upper limb with dislocated elbow, b. post-debridement, c. after soft tissue cover with Free ALT flap and skin grafting, d. 3 months post-op

Figure 3- Patient 3- a. exposed venous graft of brachial artery segmental defect, b. soft tissue coverage achieved with pedicle latissimus dorsi flap, c. post-op after the skin grafting
Discussion
The threshold for limb salvage in an upper limb is low compared to lower limb due to many reasons. The main function of the upper limb in terms of grip and prehension is far superior compared to prosthesis. The Cost, durability, and less maintenance are important factors to consider in a country like Sri Lanka. The decision to limb salvage is aided by MESS (Mangled extremity severity score) and Ganga hospital open injury score (GHOIS) (1, 2). If salvageable, the management should be in concordance with standards for the management of open fractures by British association of plastic reconstructive and aesthetic surgeons (BAPRAS) and the British Orthopaedic Association (BOA) (3). According to this evidence-based approach, proper initial assessment, antibiotics, methodical wound debridement, early soft tissue cover and rehabilitation are key aspects in patient management. The scoring systems for limb salvage can be used as an initial guide for the management but the decision should be carefully evaluated according to the expertise available in the center of management. The reported patients had a MES score of 7 and GHOI score of 16 (Grey zone) respectively. But according to the local expertise, we proceeded for limb salvage option to maximize the structural and functional outcome of the patient. The likely concern for limb salvage in this type of mangled limb is the soft tissue cover. In this type of extreme soft tissue loss, free tissue transfer by means of free flap is the key in management. Free tissue transfer should cover the non-skin graftable areas (bear bone, implants) as well as functionally important joints to maximize the range of motion.
A proper wound debridement can convert a grossly contaminated wound to a clean wound which is suitable for early internal fixation and soft tissue reconstruction without increased risk of surgical site infections. The technique of wound excision should be utilized for removal of contaminated particles rather than relying on wound irrigation alone. All the reported patients had gross contamination (Figure 1a) and clean wound beds were achieved by the debridement (Figure 1b). This facilitated the early tissue cover in patient 1(Within 48 hrs.) and early internal fixation and soft tissue cover in patient 2. None of the patients developed any surgical site infection.
Patient 3 is an example of vascular compromised mangled limb saved with brachial artery repair with venous graft and soft tissue cover achieved by pedicle latissimus dorsi flap.
Since the thumb accounts for 40% of the function of the hand, Patient 1 underwent a free 2nd toe transfer to reconstruct the right thumb. Power grip was restored with some element of opposition (Figure 1 d). He is awaiting a tenolysis to improve the range of motion of the thumb. Free tissue transfer by means of toe transfer is useful in maximizing the functional outcome of mutilated hand (4).
Recent systematic review has shown that the decision of limb salvage vs. amputation depends on many factors and most scoring systems are based on lower limb trauma (5). Until robust evidence emerges, the knowledge and the experience of the reconstructive specialist should be sought in case-by-case basis.
Conclusion.
The management of mutilating upper limb injuries poses significant challenges for all involved healthcare providers. However, it is important to prioritize upper limb salvage in patients following the stabilization of life-threatening injuries. Key steps in successful management include thorough assessment, methodical wound debridement, and prompt provision of early soft tissue coverage. Consulting with local experts is essential before considering upper limb amputation, as their insights can provide valuable guidance in decision-making processes. Furthermore, superior structural and functional outcomes are achievable through the expertise of reconstructive specialists, particularly with the use of free tissue transfers using microsurgical techniques. By adhering to these principles and engaging in collaborative decision-making, healthcare professionals can optimize patient outcomes and enhance the quality of care for individuals with mutilating upper limb injuries.
Declarations
Ethics approval and consent to participate: Not applicable
Consent for publication: Informed written consent for publication and accompanying images were obtained from the patients prior to collecting information.
Availability of data and material: All data generated or analyzed during this study are included in this published article
Competing interests: The authors declare that they have no competing interests.
Funding: The authors received no financial support for the research, authorship, and/or
publication of this article.
Authors’ contribution: Author OB, DS,PA,PN,SW,GE,TB and DD contributed to collection of information and writing of the manuscript. Author OB contributed to writing and final approval of the manuscript. All authors read and approved the final version of the manuscript
References
- Rajasekaran S, Sabapathy S, Dheenadhayalan J, Sundararajan S, Venkatramani H, Devendra A, et al. Ganga hospital open injury score in management of open injuries. European Journal of Trauma and Emergency Surgery. 2015;41(1):3-15. https://doi.org/10.1007/s00068-014-0465-9
- McNamara MG, Heckman JD, Corley FG. Severe open fractures of the lower extremity: a retrospective evaluation of the Mangled Extremity Severity Score (MESS). Journal of orthopaedic trauma. 1994;8(2):81-7. https://doi.org/10.1097/00005131-199404000-00001
- Standards for the Management of Open Fractures. Eccles S, Handley B, Khan U, Nanchahal J, Nayagam S, McFadyen I, editors: Oxford University Press; 2020 01 Aug 2020.http://DOI:10.1093/med/9780198849360.001.0001
- Georgescu AV, Battiston B, Matei IR, Soucacos PN, Bumbasirevic M, Toia F, et al. Emergency toe-to-hand transfer for post-traumatic finger reconstruction: A multicenter case series. Injury. 2019;50:S88-S94. https://doi.org/10.1016/j.injury.2019.10.056
- Nayar SK, Alcock HM, Edwards DS. Primary amputation versus limb salvage in upper limb major trauma: a systematic review. European Journal of Orthopaedic Surgery & Traumatology. 2021:1-9.https://doi.org/10.1007/s00590-021-03008-x