A patient with penetrating cardiac trauma: A real time test of integrity in the trauma care system in Sri Lanka

Abstract
Background
Management of penetrating cardiac trauma is a real time test of evaluating the integrity of a trauma care system.1 They have a low incidence of 0.16% as indicated by the trauma data bank of American College of Surgeons.2 Gunshot injuries, stab injuries and rarely accidental impalement are the main mechanisms of penetrating cardiac trauma. Knowledge and experience from high density trauma centers shows us that emergency transportation, quick response and proper diagnosis with urgent intervention is necessary to minimize fatalities.3 We present this rare case highlighting major challenges trauma care system in Sri Lanka faced with to deliver optimal care
Article
Case presentation
A teenage boy presented to a major trauma centre (MTC) after a fall from a tree of ten feet height. He was from a close by suburb and fallen directly on to a steel rod fixed to a concrete wall and it had penetrated the left side lower chest wall. He had removed the rod and was found collapsed at the scene by his elder brother. Without any further care at the scene, he was taken immediately to the close by divisional hospital which was 6km away by a trishaw (Tuk-Tuk).
The Divisional hospital has an emergency treatment unit (ETU) which caters for both trauma and non-trauma patients. It has patient monitoring facilities with a multimonitor and basic airway management devices including ambu bags, face masks and intubation facilities. Laryngeal mask airways are not available and there is no portable ventilator available. ETU is manned medical officers who are MBBS qualified. Some have undergone emergency care training and primary trauma care training.
Blood pressure was unrecordable on admission with a weak pulse and he went into cardiac arrest. With cardiac massage, ambu ventilation via face mask and one cycle of adrenaline he was resuscitated and was immediately transferred to a MTC with ambu ventilation via face mask and a Dobutamine infusion.
MTCreceived the patient approximately 40 minutes after the incident. This MTC has a separate out-patient department, trauma resuscitation bay and a short stay ward for initial assessment and observation manned by trained medical officers and nursing staff. An in-house consultant surgeon is available round the clock with or without a post graduate trainees in Surgery.
On admission, the patient was unconscious but was in sinus rhythm with a heart rate of 140 beats per minute and the blood pressure was 60/40mmHg. The patient was intubated and was connected to the portable mechanical ventilator. The puncture wound was just above the left costal margin 3cm from the left sternal edge overlying the 6th intercostal space. Bilateral air entry was equal and the heart sounds were audible with no evidence of distended neck veins.
Volume resuscitation with crystalloids and the first pint of non-crossmatched blood in the massive transfusion protocol improved the blood pressure to 100/60mmHg. An emergency focal assessment with sonography in trauma (eFAST) was performed by the radiology team at bedside using the ultrasound machine available in the MTC. .Assessment with the cardiac probe showed no evidence of cardiac tamponade and haemopneumothorax as there was malfunctioning of abdominal probe of ultrasound machine at that moment.
The radiology unit at MTC functions 24/7 under an on-call consultant radiologist with medical officers and radiographers facilitating ultrasound, X-rays and Computed Tomography (CT) scans.
Since the eFAST excluded major thoracic bleeding and there was a drop in blood pressure indicating ongoing bleeding, the bleeding was assumed to be into the peritoneal cavity with probable injury to the diaphragm. Hence, it was decided to perform an exploratory laparotomy.
Exploratory laparotomy revealed no blood in the peritoneal cavity and there was no evidence of bleeding from the diaphragm or other solid organs. As the diagnosis was in doubt, bilateral intercostal tubes were inserted and a pericardial window was created through the central tendon to exclude cardiac injury. Intercostal tubes revealed no drainage while the pericardial window revealed the presence of blood clots in the pericardial cavity.
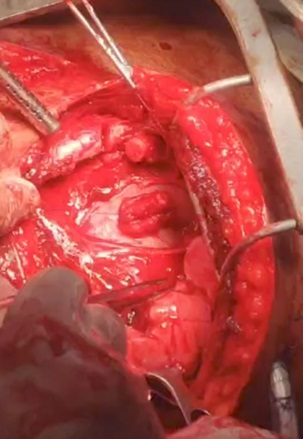
A Left anterolateral thoracotomy was performed to deal with pericardial tamponade. Bleeding from the left atrial penetrating wound was noted upon displacing pericardial blood clots. The bleeding was initially controlled with digital pressure until haemodynamic stability was achieved. The defect in the atrium was repaired using two 2-0 polypropylene stitches with pledgets. All blood clots in the pericardium were removed and pericardium was repaired using 2-0 polyglactin sutures. A pericardial drain through the pericardial window in the central tendon and a sub diaphragmatic abdominal drain was left in situ. This management was carried out by surgical and anaesthesia teams with inputs from consultant intensivist and consultant radiologist.
Figure 1: Bleeding from the defect in the atria controlled by digital pressure
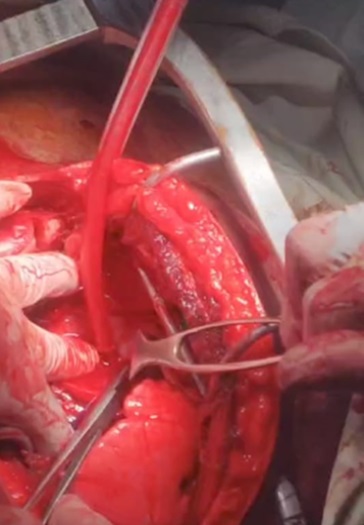
Figure 2: After the repair with pledgeted sutures
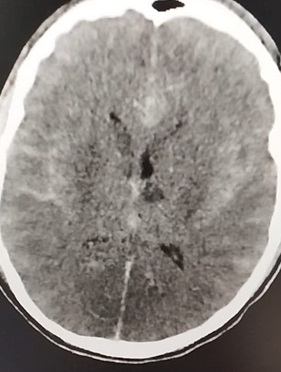
Following surgery, the patient was admitted to General Intensive Care Unit (GICU) as the MTC does not have a dedicated trauma intensive care unit nor beds reserved for trauma patients. Post-operative 2D-echocardiography showed minimal pericardial effusion with no structural defects in the heart. Despite haemodynamic stability, his neurologic status was static and his al pupils were dilated to size 4 and non-reactive by post-operative day 4. Non-contrast computer tomography revealed cerebral oedema with evidence of global ischemia. With subsequent scans and electronic encephalogram (EEG), the diagnosis of hypoxic ischaemic encephalopathy was made. On top of this, patient developed right sided pneumonia and sepsis probably as a result of aspiration The patient expired on post-operative day 18.
Figure 3: Non contrast computer tomography showing global infarction and cerebral oedema
Discussion
Penetrating cardiac injuries carry a high mortality even in world’s best trauma care systems.1 Improvement in pre-hospital care, operative management and intensive care with integrity in a trauma care system is a major factor in reducing fatalities. Management of such serious injuries gives us a good evaluation of the quality and integrity of our trauma care and an opportunity to improve the system.4,5
Sri Lanka has a free ambulance service available round the clock with trained personnel which responds to the hotline 1990.6 But this patient was taken to the hospital in a trishaw which denied him of the opportunity for pre-hospital management of airway, breathing and circulation. This signifies the need for the improvement in community awareness regarding the importance of the ambulance service and its role in prehospital care which can improve patient outcomes.
Divisional hospitals in Sri Lanka are equivalent to level III trauma centres according to the classification of American College of Surgeons – Committee on Trauma (ACS-COT).7 They have basic facilities for initial care with no specialized care, no access to radiological investigations, transfusion of blood products and theatre facilities. Their main involvement is to stabilize the patient with primary survey and immediate transfer to a nearest hospital with higher level of care.
This patient was admitted to the divisional hospital with a cardiac arrest with evidence of penetrating injury in the cardiac box. Cardiac box is the space bordered by bilateral midclavicular lines, costal margin and the clavicles in which a mediastinal injury is highly likely if there is evidence of trauma.1 An emergency room thoracotomy might have been considered at this presentation. But it was not performed in a place with bare minimum facilities and expertise.8 Thus, maintaining ventilation via a definitive airway and volume resuscitation is the maximum possible care he should have received prior to transfer going by the advanced trauma life support protocol.9 Inadequate ventilation and oxygen supply to the brain might have resulted in hypoxic injury which may have affected the final outcome.
Failure to maintain the airway was a major drawback in the initial care of this patient. To address these issues in primary trauma care, a system should be in place to constantly monitor the availability of infrastructure, resources and trained personnel. Peripheral units should be empowered to develop a trauma care using available facilities with inputs from National Trauma Secretariat. Training the staff involves getting them to follow workshops in trauma, basic life support and advance life support together with temporary attachment to higher level trauma centers. Conducting drills and refresher workshops at institutional level regularly will improve their performance in trauma care.
Communication between primary trauma care centers and field personnel with higher level centers is an important aspect of trauma care which has the capacity to improve outcomes.9 This gives the receiving centers adequate time to prepare and also an opportunity to advise on acute management. In penetrating cardiac injury, this integration of care can be an important factor in saving a life.1
This practice can be achieved simply by creating awareness among medical officers in peripheral units. Telephone communication is available island wide. Contact numbers of the personnel in higher level centers can be made available for peripheral units to be contacted in cases of emergency to inform regarding patients being transferred and to get instructions on initial management. Constructive feed back from the receiving institution regarding transferred patients and educating sending institutions without a blame culture will help to improve and maintain this practice.
A patient with a penetrating cardiac injury will present with an external entry point inside the cardiac box and haemodynamic instability. The classical triad of muffled heart sounds, hypotension and distended neck veins is rarely appreciated in the clinical setting. Options for diagnosis of a cardiac injury in an ideal setting are chest X-ray, eFAST, echocardiography and sub-xiphoid pericardial window. Sub-xiphoid pericardial window which was considered the gold standard earlier is now replaced by eFAST and echocardiography which has a high sensitivity and specificity.4,10
This patient arrived at resuscitation bay with haemodynamic instability with prior history of cardiac arrest. With initial resuscitation he was transiently stable to be taken to an operating theatre which avoided the option of emergency room thoracotomy. Only diagnostic option which was available at the bed side was the eFAST, that has a sensitivity and specificity comparable to echocardiography in identifying penetrating injury to heart and it is a crucial decision making tool in cardiac trauma algorithms around the world.1,4 The MTC did not have an institutional level cardiac trauma algorithm in place. With no evidence of haemothorax clinically and radiologically, exclusion of cardiac tamponade by the eFAST gave a suspicions of a major abdominal bleeding in the background of inaccurate assessment of peritoneal bleeding with defective ultrasound probe. Laparotomy was performed with hope of excluding abdominal bleeding and performing pericardial window to look for further evidence of cardiac tamponade.
In patients with lower thoracic or upper abdominal penetrating trauma, injuries can be in both abdomen and thorax. When adjuncts did not reveal the cause of hypotension, next step is to surgical exploration usually abdomen first as it is the site of bleeding in most cases.
In this patient blood has clotted in the pericardium which would have contributed to absence of typical appearance of pericardial effusion in eFAST scan to a certain extent. It also highlights the pitfalls of needle pericardiocentesis in this kind of situations as a preliminary measure.
Left anterolateral approach, pericardiotomy, haemorrhage control using digital pressure and atrial repair using pledgeted sutures are acceptable evidence based practices in the management of cardiac trauma4. Post operative haemodynamic stability and the echocardiography findings gave evidence for the success of the cardiac repair in the initial part.
However, it was probable that significant hypoxic insult to brain had occurred during arrest and peri-arrest period of trauma care and had contributed so much to failure of attempt at saving this patient. Dependance for ventilator and predisposition to aspiration, pneumonia and sepsis are sequalae leading to death.
Penetrating cardiac injuries carry a high mortality even in world’s best trauma care systems. Timely pre-hospital care, diagnostics and operative interventions carried out in an integrated manner is key to improve outcomes. This case highlights the importance of strengthening the trauma care system particularly related to prehospital care and diagnostics. It is also a case which demonstrates persistent clinical suspicion and logical intervention to exploration leads to achieve a correct diagnosis and treatment when investigation does not tally with clinical picture.
Acknowledgements : None
Authors’ contribution: Both authors contributed eqully
Funding : The authors received no financial support for the research, authorship, and/or
publication of this article.
Competing interests: The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Patient consent for publication: Not applicable
Ethics approval This study: Not applicable.
Data availability statement: Images are not available for patient confidentiality.
Supplemental material: Not applicable.
Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license. See: http://creativecommons.org/licenses/by-nc/4.0/.
Artificial intelligence: Generative artificial intelligence or artificial intelligence assisted technologies were not used in preparation of this article
ORCID iD
Mihira Bandara https://orcid.org/0000-0002-9548-5084
| Editor’s notes: We, the editors, hope that this mortality case report/s will help in trauma quality improvement projects (TQIP) and make it easier to come to good patient care decisions. There is no doubt that the clinical problems and systems issues presented in this case , will allow your future patients to have a better outcome.
All patient & institution identifiable information removed/changed from this article to protect privacy.
|
References
- Lee A, Hameed SM, Kaminsky M, Ball CG. Penetrating cardiac trauma. Surg Open Sci. 2023;11:45-55. doi:http://10.1016/j.sopen.2022.11.001
- Isaza-Restrepo A, Bolívar-Sáenz DJ, Tarazona-Lara M, Tovar JR. Penetrating cardiac trauma: Analysis of 240 cases from a hospital in Bogota, Colombia. World J Emerg Surg. 2017;12(1):1-7. doi:10.1186/s13017-017-0138-1
- Embrey R. Cardiac Trauma. Thorac Surg Clin. 2007;17(1):87-93. doi:10.1016/j.thorsurg.2007.02.002
- O’Connor J, Ditillo M, Scalea T. Penetrating cardiac injury. J R Army Med Corps. 2009;155(3):185-190. doi:10.1136/jramc-155-03-02
- Beard JH, Maher Z, Goldberg AJ. Penetrating Cardiac Injury. Manag Chest Trauma A Pract Guid. 2022;6(2):135-143. doi:10.1007/978-3-031-06959-8_14
- No Title. Accessed March 18, 2024. https://www.1990.lk/about-us/
- &NA; Resources for Optimal Care of the Injured Patient. Vol 7.; 2000. doi:10.1097/00043860-200007000-00002
- van Waes OJF, van Riet PA, van Lieshout EMM, Hartog DD. Immediate thoracotomy for penetrating injuries: Ten years’ experience at a Dutch level I trauma center. Eur J Trauma Emerg Surg. 2012;38(5):543-551. doi:10.1007/s00068-012-0198-6
- Kalamchi S, Harris M, Phillips JH, Loh I. Advanced Trauma Life Support.; 2022. doi:10.1142/9781800610194_0002
- Goldstein AL, Soffer D. Trauma to the heart: A review of presentation, diagnosis, and treatment. J Trauma Acute Care Surg. 2017;83(5):911-916. doi:10.1097/TA.0000000000001667